Rep. Jackie Walorski’s MIECHV Program Renews Our Commitment to Help Mothers and Babies Live Healthy Lives
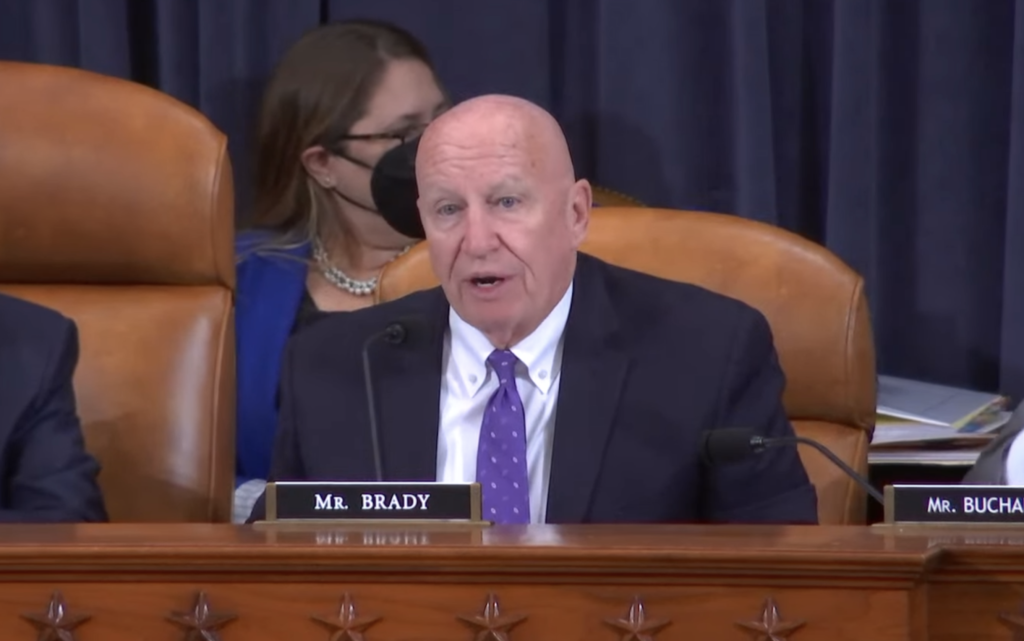
Named in honor of the late Republican Leader of the Worker and Family Support Subcommittee Rep. Jackie Walorski (R-IN), a bill to reauthorize the Maternal, Infant, and Early Childhood Home Visiting Program (MIECHV) provides stability and supports vulnerable families, Ways and Means Republican Leader Rep. Kevin Brady (R-TX) said in opening remarks for a full Ways and Means Committee hearing on MIECHV and mental health legislation.
CLICK HERE to watch.
Rep. Brady’s full remarks as prepared for delivery appear below.
Thank you, Chairman Neal.
Today we are renewing our commitment to help mothers and babies live healthy lives.
As Republican Leader of the Worker and Family Support subcommittee, our colleague Rep. Jackie Walorski made a tremendous amount of progress working with Chairman Danny Davis to move this bipartisan reauthorization forward.
I want to recognize Jackie’s family here today, her husband Dean Swihart, her mother Mert, and district staffer, Sharon Christophel, and former Indiana representative Susan Brooks.
We miss her very much and we are proud to dedicate this reauthorization of MIECHV to her. It wouldn’t be possible without her hard work as a champion for children and families.
MIECHV is a critical program that supports vulnerable families and aims to improve the health of mothers and babies through pregnancy into the early years of a child’s life.
It is a bipartisan bill and it reflects many of our Republican priorities, including increasing transparency about outcomes for families and targeting dollars to the neediest communities.
This bill would gradually increase funding from $400 million a year to $800 million a year over a five-year period, and introduce a state match as a way to expand overall service capacity across the country. The principle is simple: The federal government will invest where the states see value in investing.
It also ensures that new matching funds are allocated to states based on the number of children under five living below poverty – so funding goes where the greatest need exists.
The bill increases transparency by creating a state-by-state outcomes dashboard so we can see how interventions are impacting families, and maintains the current focus on high evidence standards.
Unlike many of our government programs, MIECHV is evidence-based – so we know the real impact on families and children and are able to direct funding toward what works.
The program has demonstrated success in supporting expecting families to increase healthy behaviors by coaching parents on child nutrition and development and mitigating risk factors to prevent child abuse and neglect.
I’m glad we found common ground with our colleagues to get this bill done, to provide stability for the program and the vulnerable families it serves.
Today we are also considering a collection of bipartisan policies that represent a step in the right direction in helping patients dealing with mental health or substance use disorders.
This bipartisan package of mental health bills will close gaps in mental health care, improve our current system to work better for patients, reduce physician burnout, protect consumers, and bring more openness into the system.
Mental health has always been an important issue, but during the pandemic, all Americans saw even greater mental health challenges as a result of COVID lockdowns and lack of access to care they needed.
Seniors and patients with commercial insurance will benefit from these improvements.
In order to address the spike in physician burnout we saw during the pandemic, we take action to protect the mental health of front line health workers by removing barriers that prevent greater access to wellness benefits.
We provide greater flexibility so that patients who need intensive treatment for mental health or substance abuse don’t have to choose between continuing to work and getting the care they need. The bill steps up outreach to ensure patients know what’s available for them.
Medicare provides options for treatment of opioid use disorder – but they’re woefully underutilized. This bill steps up outreach to ensure patients know what’s available to them.
And for better consumer protection and transparency, we build on improvements in the No Surprises Act by requiring providers to inform health plans if they’re accepting new patients.
Victims of sexual assault will be protected from cost-sharing associated with treatment and exams related to their assault.
With that, Mr. Chairman, I yield back.
Thank you.